
trigger finger
introduction
Trigger finger, medically known as stenosing tenosynovitis, is a condition that causes one or more fingers to become stuck in a bent position before snapping straight, much like pulling and releasing a trigger. This occurs due to inflammation and narrowing of the tendon sheath in the affected finger, making movement difficult and sometimes painful.
While trigger finger is not life-threatening, it can severely impact daily activities, grip strength, and hand function, especially for people who rely on fine motor skills, such as musicians, typists, and manual laborers. Left untreated, it may lead to permanent stiffness and reduced hand mobility.
This article explores the causes, symptoms, risk factors, diagnosis, treatment options, and the role of physiotherapy in managing trigger finger, with a special focus on home-based recovery and rehabilitation.
causes of trigger finger
Trigger finger occurs when the flexor tendon in the affected finger becomes inflamed or irritated, leading to thickening and the formation of nodules that restrict smooth movement through the tendon sheath. Some of the most common causes include:
- Repetitive Hand Movements – Frequent gripping, pinching, or flexing of fingers (e.g., prolonged use of tools, typing, or playing musical instruments).
- Tendon Inflammation or Swelling – Conditions like tenosynovitis, where the tendon lining becomes inflamed, increasing friction in the sheath.
- Scar Tissue Formation – Previous hand injuries or surgeries can lead to scar tissue, restricting tendon movement.
- Hormonal Changes – People with hormonal imbalances, such as in diabetes or thyroid disorders, have a higher risk of developing trigger finger.
- Aging – Natural wear and tear over time can make tendons less flexible and more prone to thickening.
symptoms of trigger finger
The severity of symptoms can vary, from mild discomfort to severe immobility of the affected finger. Some common symptoms include:
- Finger stiffness, especially in the morning.
- Clicking or popping sensation when bending or straightening the finger.
- Pain and tenderness at the base of the affected finger or thumb.
- Locking of the finger in a bent position, which may suddenly pop straight.
- A palpable nodule near the base of the affected finger.
In severe cases, the finger may become completely stuck in a bent position, requiring manual assistance to straighten.
risk factors for trigger finger
Certain individuals are more prone to developing trigger finger due to lifestyle habits, medical conditions, or occupational hazards. Key risk factors include:
- Repetitive Hand Use: People who frequently grip tools, use keyboards, or play musical instruments are at higher risk.
- Diabetes & Rheumatoid Arthritis: Chronic inflammation and poor circulation can contribute to thickening of the tendons.
- Gender: Women, particularly those aged 40-60, are more likely to develop trigger finger due to hormonal fluctuations.
- Hand Trauma or Surgery: Prior injuries or surgeries on the hand can lead to scar tissue buildup, increasing friction.
- Carpal Tunnel Syndrome: Patients who have undergone carpal tunnel surgery may be more susceptible to trigger finger.
Understanding these risk factors allows individuals to take preventive measures before symptoms worsen.
diagnosis of trigger finger
Diagnosing a trigger finger usually involves a physical examination rather than advanced imaging tests.
Steps in Diagnosis:
- Patient History: The doctor will ask about hand usage, symptoms, and any past injuries or conditions.
- Physical Examination:
- Checking for stiffness, clicking, or nodules at the base of the affected finger.
- Assessing whether the finger locks in a bent position and if manual force is needed to straighten it.
- Imaging Tests (if needed):
- Ultrasound or MRI may be used in rare cases to check for tendon damage or inflammation.
Early diagnosis ensures timely treatment and prevents long-term complications.
treatment options for trigger finger
The goal of treatment is to reduce inflammation, relieve pain, and restore smooth finger movement. Treatment options range from conservative methods to surgical interventions, depending on the severity of the condition.
1. Non-Surgical Treatments
Rest & Activity Modification
- Avoid repetitive gripping or prolonged hand strain to allow the tendon to heal.
Splinting
- Wearing a finger splint at night keeps the finger in a straight position, preventing stiffness and reducing strain.
Medications
- NSAIDs (Ibuprofen, Naproxen): Help reduce pain and inflammation.
- Steroid Injections: Corticosteroid injections directly into the affected tendon sheath can provide temporary relief by reducing swelling.
Physiotherapy & Stretching
- Gentle stretching exercises can help loosen the tendon sheath and improve mobility.
2. Surgical Treatment (For Severe Cases)
If conservative treatments fail, surgery may be needed. The most common procedures include:
- Percutaneous Release – A needle is used to release the constricted tendon sheath.
- Open Surgery – A small incision is made to manually free the tendon.
Most patients recover fully within a few weeks to months with proper post-surgical care and rehabilitation.
role of physiotherapy in trigger finger recovery
Physiotherapy plays a crucial role in both non-surgical management and post-surgical rehabilitation for trigger finger. Key benefits include:
1. Improving Finger Mobility & Strength
- Stretching & Range of Motion Exercises prevent stiffness and promote smooth movement.
- Strength training enhances grip strength and hand coordination.
2. Reducing Pain & Inflammation
- Ultrasound Therapy & Massage Techniques help improve blood circulation and reduce inflammation.
3. Preventing Recurrence
- Physiotherapists guide patients on ergonomic modifications and hand positioning techniques to prevent reinjury.
Regular physiotherapy sessions ensure faster recovery and long-term relief.
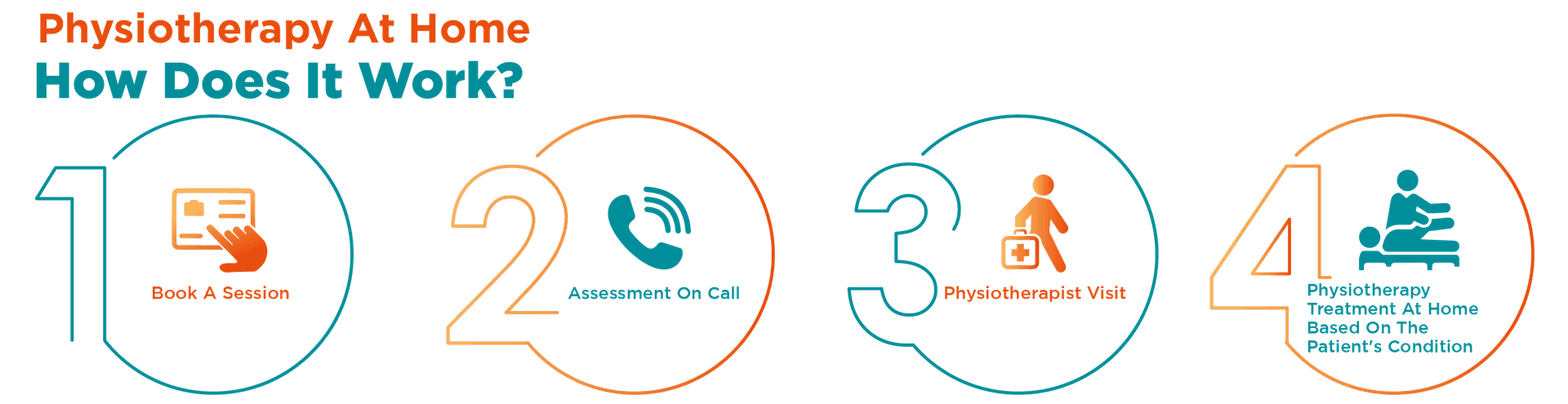
how portea supports trigger finger recovery
At Portea, we provide expert physiotherapy services to help patients recover from trigger finger and regain normal hand function—all in the comfort of their homes. Our comprehensive physiotherapy extends beyond trigger finger treatment, covering a wide range of rehabilitation services, including post-surgical recovery, arthritis management, neuro-rehabilitation, sports injury rehabilitation, orthopedic care, elderly physiotherapy, and respiratory therapy. With our dedicated team of experienced physiotherapists, we ensure that each patient receives personalized, professional care to enhance recovery, restore mobility, and improve overall quality of life.
conclusion
Trigger finger may seem like a minor condition at first, but if left untreated, it can severely impact hand function and quality of life. Early diagnosis, lifestyle modifications, physiotherapy, and, if necessary, surgical intervention can help restore normal finger movement.
Taking proactive steps—such as avoiding repetitive strain, performing hand stretches, and seeking professional physiotherapy—can prevent long-term complications. Whether you are recovering from a trigger finger or post-surgical treatment, Portea’s home-based physiotherapy services ensure a smooth and comfortable rehabilitation process.
Don’t let finger pain hold you back—take action today for a pain-free tomorrow!
faqs
1.Can trigger finger be prevented?
Preventive measures include avoiding repetitive gripping, stretching exercises, using ergonomic tools, and taking breaks during hand-intensive activities. Managing conditions like diabetes and arthritis also helps reduce the risk of developing trigger finger over time.
2.Is surgery necessary for a trigger finger?
Surgery is only required when conservative treatments like splinting, medications, and injections fail to relieve symptoms. The procedure releases the tightened tendon sheath, allowing smooth finger movement and preventing further locking or stiffness.
3.How long does recovery take after trigger finger surgery?
Recovery typically takes a few weeks. Physical therapy and hand exercises help restore strength and movement. Mild discomfort and swelling may persist initially, but most patients regain full function within a few months with proper post-surgical care.
4.Can the trigger finger heal on its own?
Mild cases may improve with rest, stretching, and lifestyle adjustments. However, persistent cases often require medical treatment, such as steroid injections or splinting, to prevent worsening and restore normal finger movement without long-term stiffness or pain.
5.Who is at risk of developing trigger finger?
People performing repetitive hand movements, those with diabetes, rheumatoid arthritis, or manual laborers are at higher risk. Women over 40 are also more prone due to hormonal changes affecting tendon flexibility and inflammation levels.
6.Does trigger fingers affect multiple fingers?
Yes, it can affect one or multiple fingers, including the thumb. Some people experience it in both hands simultaneously, especially if they engage in repetitive hand activities or have underlying conditions like diabetes or rheumatoid arthritis.
Doctor Consultation
Nursing
Physiotherapy
Trained Attendant
Elder Care
Mother & Baby Care
Lab Tests
Medical Equipment
Speciality Pharma
Critical Care






