tenosynovitis
introduction
Tenosynovitis is a condition that involves inflammation of the sheath surrounding a tendon, leading to pain, swelling, and restricted movement. This condition often affects the hands, wrists, and feet but can occur in any tendon sheath. It is commonly caused by repetitive motion, overuse, infection, or underlying medical conditions such as rheumatoid arthritis. If left untreated, tenosynovitis can lead to chronic pain and limited function, impacting daily activities. Early intervention and appropriate management strategies can help alleviate symptoms and prevent complications.
recognizing the warning signs of tenosynovitis
The primary symptom of tenosynovitis is pain and tenderness along the affected tendon, which may worsen with movement. Swelling and redness around the area are also common indicators. Many individuals report a feeling of stiffness, particularly in the morning or after periods of inactivity. In some cases, crepitus (a grinding sensation) may be felt when the tendon moves. If the condition progresses, difficulty in moving the affected joint and a locking sensation can develop. Severe cases may result in infection, requiring immediate medical attention.
understanding the causes of tenosynovitis
Tenosynovitis can result from various factors, with the most common being repetitive strain or overuse of a tendon. Other causes include:
- Injury or trauma: Direct impact or strain on a tendon can lead to inflammation.
- Inflammatory conditions: Diseases like rheumatoid arthritis and gout can trigger tendon sheath irritation.
- Bacterial infections: Puncture wounds or open injuries can introduce bacteria, leading to infection.
- Repetitive movements: Occupations requiring frequent hand or wrist motions increase the risk.
- Poor ergonomics: Incorrect posture or excessive strain on tendons can contribute to the condition.
Identifying the underlying cause is essential for effective treatment and prevention of recurrence.
who is at risk?
Certain individuals are more prone to developing tenosynovitis. Risk factors include:
- Repetitive hand or wrist movements: Common among typists, assembly line workers, and musicians.
- Inflammatory diseases: Conditions like rheumatoid arthritis or lupus increase susceptibility.
- Athletes: Sports involving repetitive strain, such as tennis and running, can lead to inflammation.
- Diabetes: This condition heightens the risk of tendon-related problems.
- Direct trauma: Injuries to the affected area can trigger inflammation.
Recognizing these risk factors can help in early diagnosis and preventive care.
how to reduce the risk of tenosynovitis
Preventing tenosynovitis involves lifestyle adjustments and ergonomic modifications. Some effective preventive measures include:
- Taking regular breaks: Avoiding prolonged repetitive activities to reduce tendon strain.
- Using ergonomic equipment: Maintaining proper posture and utilizing supportive tools at work.
- Stretching and strengthening exercises: Enhancing flexibility and promoting tendon health.
- Avoiding excessive force: Reducing unnecessary stress on tendons during physical activities.
- Prompt infection treatment: Addressing bacterial infections to prevent tendon sheath irritation.
By adopting these practices, individuals can significantly lower their risk of developing tenosynovitis.
diagnosis and treatment approaches for tenosynovitis
Tenosynovitis is diagnosed through physical examination, patient history, and imaging tests such as ultrasound or MRI to assess tendon inflammation. Treatment focuses on relieving pain and reducing inflammation. Common approaches include:
- Rest and immobilization: Limiting movement to promote healing.
- Cold and heat therapy: Alternating ice packs and warm compresses to reduce swelling and stiffness.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) help manage pain and inflammation.
- Physiotherapy: Stretching and strengthening exercises to restore tendon flexibility and function.
- Corticosteroid injections: Used in severe cases to alleviate persistent inflammation.
- Surgery: Rarely required but may be necessary to release a constricted tendon sheath.
Early treatment can prevent chronic pain and long-term mobility issues.
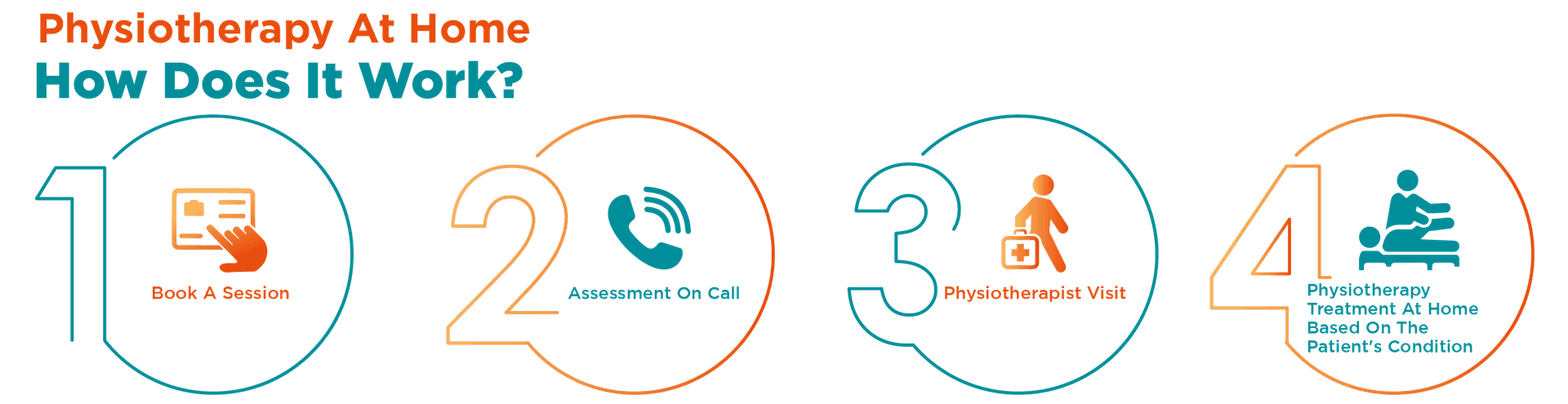
physiotherapy: a key component of care
Physiotherapy plays a crucial role in the recovery and management of tenosynovitis. Skilled physiotherapists utilize techniques such as manual therapy, ultrasound therapy, and guided exercises to improve tendon mobility and reduce pain. Additionally, they educate patients on ergonomic corrections and preventive exercises to minimize future strain. Physiotherapy not only accelerates healing but also helps restore functionality, ensuring a smoother recovery process.
how portea supports tenosynovitis management
At Portea, we recognize the challenges faced by individuals with tenosynovitis and offer personalized home-based physiotherapy services to support their recovery. Our expert physiotherapists focus on helping patients regain strength, mobility, and independence in a comfortable home setting.
Beyond tenosynovitis management, we specialize in a range of physiotherapy services, including post-surgical rehabilitation, arthritis care, neuro-rehabilitation, sports injury recovery, orthopedic care, elderly physiotherapy, and respiratory therapy—all delivered at home for maximum convenience. With our dedicated and experienced team, we ensure that each patient receives professional, customized care to enhance their recovery and improve their quality of life.
faqs
1.Can tenosynovitis be prevented?
Yes, prevention includes avoiding repetitive strain, using proper posture, strengthening muscles, and taking breaks during repetitive activities. Wearing supportive braces and practicing stretching exercises can help maintain tendon flexibility and reduce the risk of inflammation.
2.Is tenosynovitis a serious condition?
While not life-threatening, untreated tenosynovitis can lead to chronic pain, reduced mobility, and permanent tendon damage. Early treatment is crucial to prevent complications and restore normal function. Severe cases may require surgical intervention.
3.How long does tenosynovitis take to heal?
Mild cases improve within a few weeks with rest and treatment, while severe cases may take months. Chronic conditions may require long-term therapy. Recovery time depends on severity, treatment effectiveness, and whether repetitive strain is avoided.
4.Can tenosynovitis come back after treatment?
Yes, recurrence is possible if the underlying cause, such as repetitive motion or poor ergonomics, isn’t addressed. Strengthening exercises, proper posture, and avoiding excessive strain on tendons can help prevent flare-ups and long-term complications.
5.When should I see a doctor for tenosynovitis?
Consult a doctor if pain, swelling, or stiffness persists despite rest and home treatment. Immediate medical attention is needed if symptoms worsen, movement becomes severely restricted, or there are signs of infection like redness, warmth, and fever.
Doctor Consultation
Nursing
Physiotherapy
Trained Attendant
Elder Care
Mother & Baby Care
Lab Tests
Medical Equipment
Speciality Pharma
Critical Care






